Announcement
Virtual Solutions for Mental Health Improve Symptoms and Expand Access, but Some Tools Come with High Costs
NEW YORK —
A new evaluation from the Peterson Health Technology Institute (PHTI) indicates that virtual solutions for depression and anxiety can meaningfully improve outcomes for people with mild-to-moderate symptoms, but current pricing models for some result in higher total healthcare costs for employers and plans.
Mental health conditions like depression and anxiety affect one in five U.S. adults, and timely access to care remains a challenge because of provider shortages, long wait times, and affordability barriers. PHTI reviewed a range of virtual solutions that include on-demand digital content and activities, which can be used on their own or in combination with therapy and medication. The evaluation finds that these solutions expand access and are particularly effective for people who are not otherwise receiving therapy.
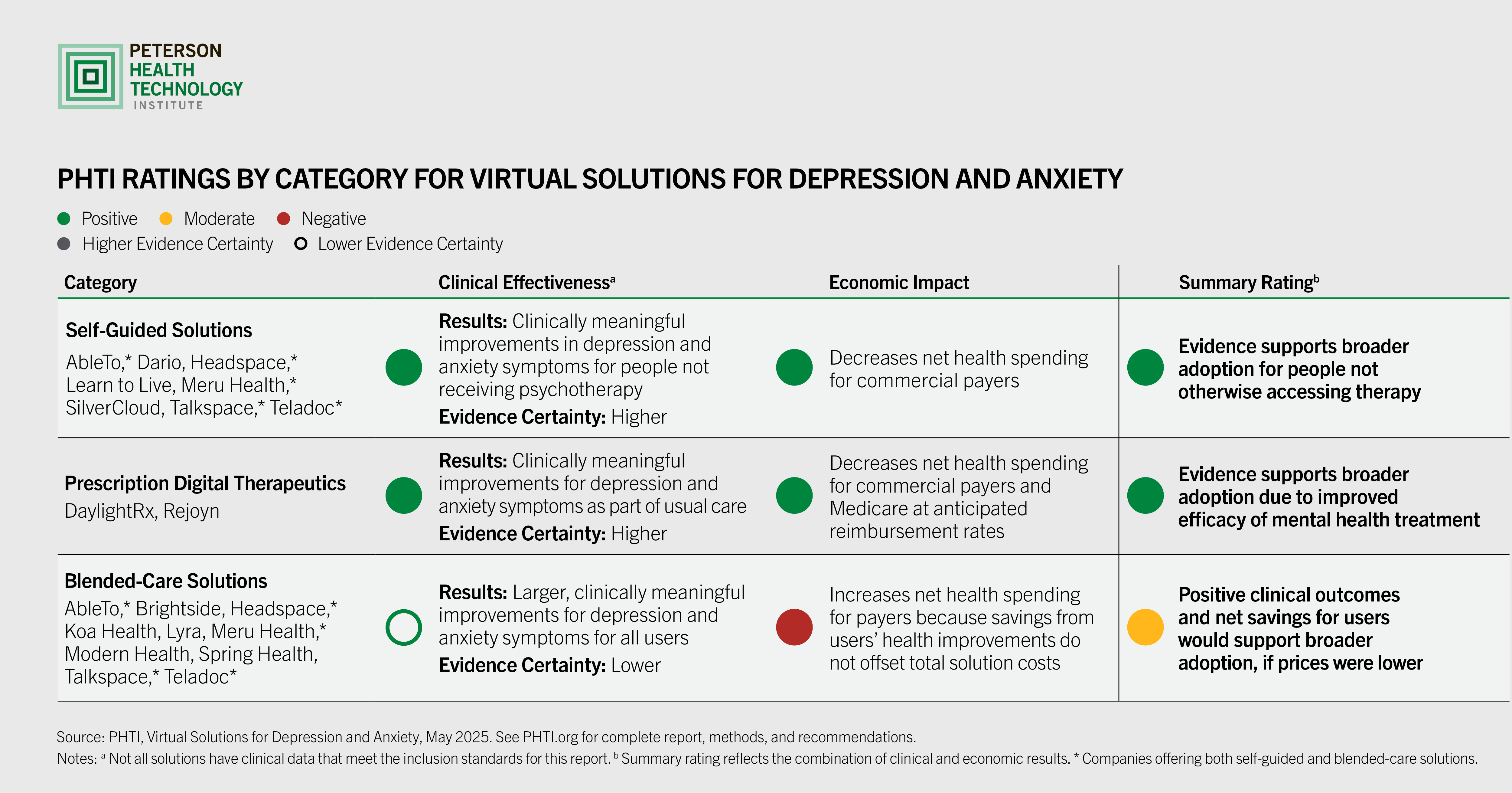
PHTI evaluated three categories of solutions that employers, health plans, and providers are increasingly adopting:
- Self-guided solutions, which offer digital content that people can access anytime;
- Prescription digital therapeutics,which are U.S. Food and Drug Administration-cleared digital programs that require a prescription from a doctor or therapist; and
- Blended-care solutions, which have networks of virtual care teams that integrate therapy and digital content.
PHTI’s evaluation finds important differences in clinical outcomes and economic impact across these approaches:
- Evidence supports broad adoption of self-guided solutions to expand access to mental healthcare, because these tools produce meaningful clinical benefits for users who are not otherwise receiving therapy. At relatively low price points, these solutions can also reduce total healthcare spending for commercial payers.
- Prescription digital therapeutics that are used in conjunction with other treatment can improve the efficacy of mental healthcare for depression and anxiety symptoms. These solutions warrant broader adoption at anticipated reimbursement rates and could deliver additional savings if they are used to reduce the frequency or duration of therapy.
- Blended-care solutions, which comprise the largest share of this market, appear to have even more meaningful clinical benefits for users compared with self-guided solutions or prescription digital therapeutics and reduce healthcare costs for users. However, current pricing models that charge an access fee for all employees (regardless of whether they use the solution) result in overall increases in net health spending by employers and health plans. Because these solutions show clinical benefits and net health savings for individual users, they could be adopted more broadly if prices were lower or fees were charged only for people who use the solution.
“Virtual solutions for depression and anxiety can expand access to care by offering a range of convenient, affordable, and effective treatment options,” said Caroline Pearson, executive director of PHTI. “Employers that offer these solutions as part of their benefits package can see lower healthcare spending per user and improved productivity. However, to manage total overall costs, employers must negotiate lower prices for blended-care solutions and help guide users to more affordable treatment options when appropriate.”
Depression and anxiety are two of the most common mental health conditions in the United States. Rates of depression and anxiety have steadily increased over the past decade and sharply spiked during the COVID-19 pandemic. Nationally, these disorders carry a significant economic burden, both in direct treatment costs and in indirect costs, such as lost productivity and absenteeism. Approximately $240 billion was spent in the United States on these two mental health disorders in 2020.
Large employers and health plans are increasingly adopting virtual depression and anxiety solutions to address rising unmet care needs. More than half (56%) of purchasers surveyed in PHTI’s 2024 State of Digital Health Purchasing survey said they offered or covered mental health solutions in the past two years, and that mental health remains a priority in the year ahead.
“Purchasers have ways that they can make these virtual solutions for mental health more effective, efficient, and tailored to patients. They can seek solutions offering lower per-member-per-month costs, integrate solutions into employee assistance programs to offset costs, and work with vendors to right-size solutions based on employees’ needs,” said Pearson.
PHTI evaluated 15 virtual depression and anxiety offerings from public and private companies, including: Amwell (SilverCloud), Big Health (DaylightRx), Brightside Health, DarioHealth, Headspace, Koa Health, Learn to Live, Lyra Health, Meru Health, Modern Health, Optum (AbleTo), Otsuka Precision Health (Rejoyn), Spring Health, Talkspace, and Teladoc Health.
PHTI’s evaluation is based on its independent assessment framework, which evaluates the clinical and economic benefits of digital health solutions. For this report, PHTI reviewed more than 5,000 articles and other evidence, including information submitted by companies with solutions included in the report. PHTI partnered on the report with clinical advisors and experts in health technology, health economics, psychology, psychiatry, and behavioral sciences. The report also included interviews with people with depression and anxiety who use digital health solutions.
###
About the Peterson Health Technology Institute
The Peterson Health Technology Institute (PHTI) provides independent evaluations of innovative healthcare technologies to improve health and lower costs. Through its rigorous, evidence-based research, PHTI analyzes the clinical benefits and economic impact of digital health solutions. These evaluations inform decisions for providers, patients, payers, and investors, accelerating the adoption of high-value technology in healthcare. PHTI was founded in 2023 by the Peterson Center on Healthcare. For more information, please visit PHTI.org