Announcement
Virtual Opioid Use Disorder Solutions Are as Effective as Usual Care, but Only Slightly Improve Retention
NEW YORK —
A new evaluation from the Peterson Health Technology Institute (PHTI) indicates that virtual solutions for opioid use disorder (OUD) are as effective as usual, medication-based treatment and can help people stay in treatment slightly longer. However, despite growing investment in and adoption of these digital solutions, there is no clear evidence that they meaningfully reduce the overall cost of care or expand participation in OUD treatment.
The evaluation finds that people using virtual OUD solutions remain in treatment an average of 13 more days over six months, only slightly longer than usual care. Usual care includes treatment with medications such as buprenorphine, naltrexone, and methadone, often combined with counseling and recovery support. Evidence shows that treatment retention is the critical factor for clinical effectiveness because patients who remain in treatment have lower risk of fatal overdose and fewer emergency department visits and hospital admissions. Given that these solutions only slightly improve treatment retention compared with usual care, they do not substantially reduce healthcare spending and may increase costs, depending on the solution’s price.
Despite expectations that virtual solutions would expand the number of people in medication-based OUD treatment by improving access to care and convenience, the assessment found no increase in the number of patients initiating treatment.
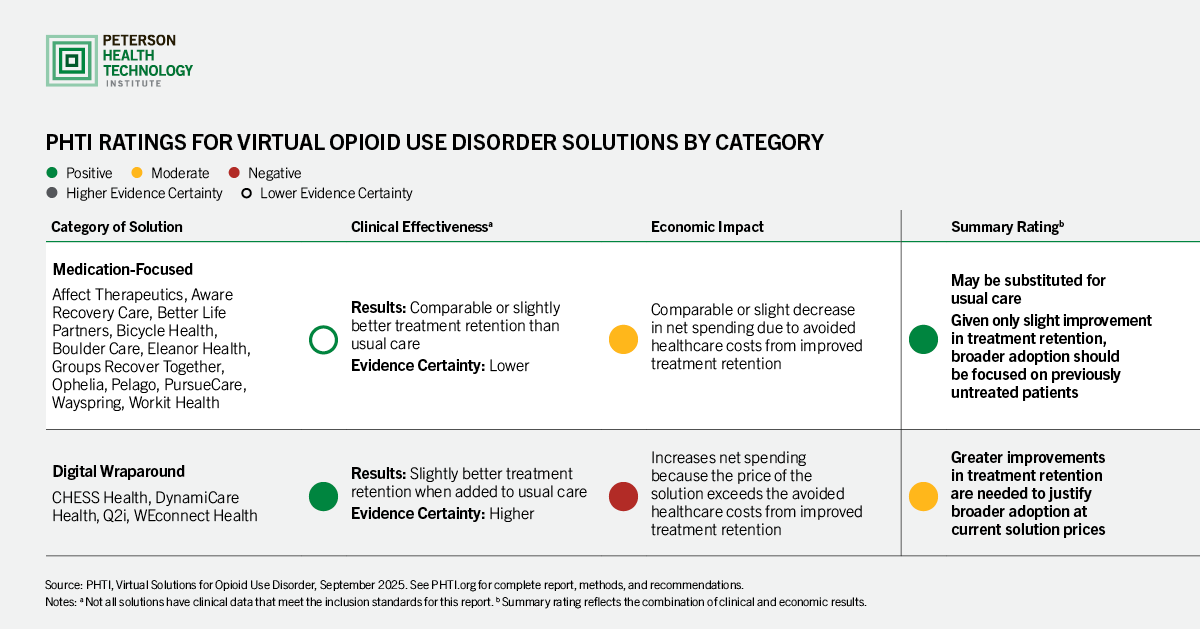
PHTI evaluated two types of solutions that employers, providers, health plans, Medicaid programs, and public health agencies purchase:
- Medication-focused solutions, which offer virtual prescribing and optional therapy, peer support, or other digital content; and
- Digital wraparound solutions, which are added to usual care and offer support services such as contingency management, peer support, and care navigation for those in existing treatment programs.
PHTI’s evaluation finds medication-focused solutions may be substituted for usual care, but there is no evidence that these solutions substantially improve clinical outcomes, reduce net costs, or expand access to care. Purchasers can expect comparable or slightly lower spending for these medication-focused solutions compared with in-person care, because slightly greater treatment adherence can mitigate some costs associated with hospitalizations and emergency department visits.
Evidence shows that digital wraparound solutions increase net spending for purchasers because the solution prices exceed avoided healthcare costs from improved treatment retention. According to the assessment, broader adoption of these solutions could be justified if new evidence showed that they help people stay in treatment longer.
“When it comes to opioid use disorder, any additional time in treatment helps patients avoid relapse and overdose risk. Virtual solutions perform as well as or slightly better than traditional care models, but healthcare providers and digital solutions need to continue striving for interventions that deliver more substantial improvements in retention and effectiveness,” said Caroline Pearson, executive director of PHTI. “In the meantime, the biggest impact for these solutions is to expand adoption to previously untreated patients who can benefit from proven medications and desperately need the help.”
OUD remains a significant public health crisis, affecting more than 9 million adults across the United States and contributing to approximately 80,000 deaths from overdose each year. The United States spends $111 billion annually on direct healthcare costs for people with OUD and an additional $52 billion on related criminal justice costs. More than 75% of employers say they have employees who have been affected by opioid use, and one-third report feeling unprepared to help employees manage the condition, particularly those in industrial, construction, and transportation occupations.
Only one in four adults with OUD who would benefit from medication-based treatment receive it. Barriers to care include limited provider availability, high costs, complex public policies governing telehealth and controlled substances, and social stigma. The Centers for Disease Control and Prevention also estimates that 95% of people living with OUD who are not receiving treatment do not believe they need it.
PHTI evaluated 16 virtual OUD solutions from private companies, including: Affect Therapeutics, Aware Recovery Care, Better Life Partners, Bicycle Health, Boulder Care, CHESS Health, DynamiCare Health, Eleanor Health, Groups Recover Together, Ophelia, Pelago, PursueCare, Q2i, Wayspring, WEconnect Health, and Workit Health.
The report provides recommendations for purchasers, innovators, and policymakers, including:
- Generate more evidence about what tools work and for whom
- Expand access by bringing more untreated patients into treatment and keeping them in treatment longer
- Use opioid settlement funds to promote evidence-based treatment approaches
- Modernize teleprescribing policies at the federal and state levels
PHTI’s evaluation is based on its independent assessment framework, which evaluates the clinical and economic benefits of digital health solutions. For this report, PHTI reviewed more than 4,800 articles and other evidence, including information submitted by companies with solutions included in the report. PHTI partnered on the report with clinical advisors and experts in health technology, health economics, addiction medicine, psychiatry, and internal medicine. The report also included interviews with people with OUD who use digital health solutions.
###
About the Peterson Health Technology Institute
The Peterson Health Technology Institute (PHTI) provides independent evaluations of innovative healthcare technologies to improve health and lower costs. Through its rigorous, evidence-based research, PHTI analyzes the clinical benefits and economic impact of digital health solutions. These evaluations inform decisions for providers, patients, payers, and investors, accelerating the adoption of high-value technology in healthcare. PHTI was founded in 2023 by the Peterson Center on Healthcare. For more information, please visit PHTI.org